BM(Hons) MD FRCS(Neurosurgery)
Consultant Neurosurgeon
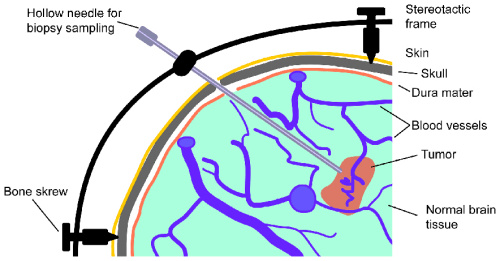
A biopsy is an operation in which a needle is passed into a tumour to take small samples to send for analysis in order to determine a precise diagnosis.
Image-guided refers to the use of scans and a computer to precisely locate and target a lesion within the brain. This was previously commonly done by fixing a metal frame to the head with pins and carrying out a (CT or MRI) scan with the frame on (frame-based stereotaxy). Nowadays your scan can be performed in advance of your surgery (without a frame on), the data is uploaded onto a computer in the operating room, and a navigation system is used to locate the tumour (frameless stereotaxy or image-guidance).
A biopsy is usually performed because your scans have shown a lesion in the brain. Unfortunately, these scans are only about 60-70% reliable in diagnosing different types of lesion within the brain. A biopsy is needed to be certain of the diagnosis so that we can plan the best treatment for you and give you more accurate information on prognosis.
You do not usually need to have a general anaesthetic but will be given some sedation. In the operating theatre you will be positioned on an operating table and your head will be supported on a headrest. A neuronavigation system (like a satellite navigation system) will then be used together with your pre-operative scan data to precisely locate the site for the biopsy (target) and to determine an entry point, which can then be marked on the scalp. A small incision can then be marked on the scalp and a very small amount of hair shaved along the line of the incision before it is cleaned with antiseptic solutions and then surrounded by surgical drapes. A small injection of local aneasthetic is used to numb the incision site: this stings for a few seconds only. Nothing else should hurt at all.
An incision is then made and a special drill used to create a burr hole approximately 14mm in diameter - this is a bit noisy for a few seconds. A small device is then screwed to the bone edges to hold the biopsy needle in position. Using the navigation system the trajectory for the biopsy needle is planned and the biopsy needle is then passed into the tumour and a series of biopsies are taken. The wound is then closed with stitches and staples for the skin.
You will be transferred to the recovery area for a short time and then to the neurosurgery day-case unit where observations will be performed regularly. This will include an assessment of your conscious level (asking you to follow simple commands, opening your eyes and answering questions), examination of your pupil responses, tests of your limb strength and checks on your pulse, blood pressure and respirations. After 4 hours you will have a CT scan of the head before your discharge after about 6 hours (either home or back to your local hospital). Occasionally it is necessary to stay in for longer.
A biopsy is not particularly painful but you will be given some tablets for any headaches and if you feel nausea you will be given drugs to relieve this symptom. You will often be given steroids to prevent swelling (in a slowly reducing dose) and anti-epileptic drugs to prevent fits in the early post-operative period. You can eat, drink and mobilise as soon as you feel able to, which is usually within a few hours of surgery.
Your surgeon will arrange an appointment with you to discuss the results of the biopsy, usually 5-7 days after surgery. The staples can be removed from your wound at 5 days, usually at your post-op appointment and you can wash your hair after this time. Your surgeon will also explain to you any plans for further treatment and follow-up.
You may have some mild headaches, which will lessen with time and you may feel tired and need to rest at home. If you are taking steroids, the dose will slowly be reduced, as prescribed by your surgeon, and if you have not had any fits your anticonvulsants will be stopped, as directed by your surgeon.
You will not be able to drive for a time determined by your symptoms and diagnosis. You should inform the DVLA of your diagnosis and give them the name of your treating surgeon by calling 0870 2400009. They will send a form to your surgeon for him to complete and will then inform you of the date on which you may return to driving. For further information, the DVLA's guidelines are published on-line at http://www.dvla.gov.uk/welcome.htm. Because of the small risk of a fit, you should also avoid any other activities that may put you at risk if you were to suffer a brief loss of consciousness, such as, climbing ladders, operating certain machinery or swimming unsupervised.
Every operation carries a risk. Overall, complications following a biopsy are rare and the degree of risk depends on a number of factors, for example, location and type of the tumour, your general medical health and age. Your surgeon will explain to you the particular risks associated with your operation and give you an indication of the likely chance of complications occurring. Complications include, but are not exclusive to, the following:
Some of these complications might be serious enough to warrant further surgery and some can be life threatening. Overall, as a general guide, the incidence of serious complications causing severe permanent neurological deficit (stroke) or death is about 2%.
Very occasionally the tiny samples of tissue will not be sufficient to give a definite diagnosis and the operation may need to be repeated. This happens to about 1% of patients, therefore, there is a 99% chance that the operation will give a diagnosis. Some primary brain tumours may not be the same all the way through and there is a small chance, therefore, that a small biopsy is not fully representative of the whole tumour. This could lead to the tumour being incorrectly graded (too low). We try to avoid this sampling error by taking several biopsies from different locations from the tumour and by targeting the most abnormal areas on the scan.
No. The aim of the operation is to obtain a diagnosis in order to plan your future treatment and to be able to give you an indication of prognosis.